Course Overview
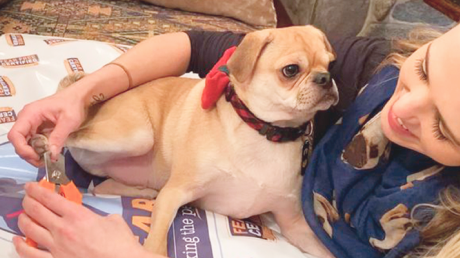
For humans, nail trims are mundane experiences. But for pets, nail care can cause stress by imposing on their personal space, restricting their freedom to move, and sometimes causing discomfort or even pain.
Successful nail care encompasses more than just being able to physically maintain nails. True success is found in gaining calm participation and trust from the animals you’re working with.
This course will teach you to:
- View nail care from the pet’s perspective and identify several common causes of FAS
- Understand the uses, benefits and drawbacks of each common nail trim tool: clippers, nail grinders, nail files, and scratch boards
- Incorporate the Fear Free concepts of Gentle Control, Considerate Approach and touch gradient into nail care
- Describe how, and just as importantly, when, to use food distractions, desensitization and classical conditioning, or consider medications to achieve Fear Free nail trims
This one-hour course is open to all professionals who are signed up for a Fear Free certification program and is approved for 1 RACE CE hour and one hour of CEUs from CCPDT, IAABC and KPA
This course consists of four lessons:
- Lesson 1: Nails, from the Pet’s Perspective
- Lesson 2: Tools of the Trade
- Lesson 3: Applying Fear Free Core Concepts to Nail Care
- Lesson 4: Going Beyond Food Distractions

His official title is Community Outreach TNVR Coordinator, but most of the time, Paul Bates feels like a mediator, problem solver, and teacher. That suits him just fine.
Bates leads the team at Peggy Adams Rescue League in West Palm Beach, Florida. The organization works closely with shelter volunteers, cat rescue groups, and cat-caring neighbors to ensure free-roaming cats in Palm Beach County are properly vaccinated, sterilized, and fed.
It is estimated that more than 200,000 cats live on the streets in Palm Beach County. Once called feral cats, they are now identified as community cats.
“These are cats who live outside, who do not belong to anybody, and who are not adoptable because they are not socialized with people,” says Bates. “They certainly do not belong in animal shelters where they are often euthanized. Our job is to work with community cat advocates to make sure these community cats are neutered/spayed, vaccinated, and returned to their outdoor homes.”
On the Case
It’s a tall order, but Bates is up for the challenge. He is a Fear Free Pets Shelter Course graduate who works to educate people about the mindset of community cats and safe ways to trap, vaccinate, spay/neuter, and return these cats back to their colonies without stressing them or getting injured.
His shelter also helped get a county-wide law adopted that requires these cats to be sterilized, vaccinated, implanted with a microchip, have left ears clipped to identify these actions and then released to the same area where found.
Bates makes daytime and night-time visits to community cat sites in neighborhoods, car dealership parking lots, and alleys behind restaurants. He gives talks to volunteers and shares tips and resources on two key Facebook pages: Project CatSnip and Community Cats of the Palm Beaches. Project CatSnip is a program of the Peggy Adams Rescue League that provides free TNVR through grant funding and conducts free humane trapping classes.
Safety 101
Even though many of these cats appear friendly and may even allow a trusted person who feeds them to pet them, they are still capable of lashing out if they feel threatened.
“If you see a stray, friendly cat, do not attempt to pick up the cat and put him in a carrier because chances are that you will be bit or scratched,” he cautions. “Scooping up a cat in your arms can make them go into panic mode. The nails come out, and the teeth are ready to bite. It is far safer to set up humane traps to get them in so we can give them vaccinations and spay/neuter them and return them to their cat colony.”
To reduce fear or anxiety in the cat during transport, Bates recommends placing bed linens made of breathable fabric over the trap to help the cat settle down.
“A cat in an uncovered trap is apt to freak out and bounce off the sides of the cage,” he says. “Covered humane traps look like safe spots to a cat. Avoid using heavy blankets, thick towels or quilts because a cat inside could overheat due to the lack of air flow. And, he could also have to inhale the strong ammonia smell if he urinated or defecated during transport.”
To reduce fleas and ticks among these community cats, Bates recommends mixing food-grade diatomaceous earth powder with catnip and allowing the free-roaming cats to roll in it. This powder is safe for pets and people, but destroys exoskeletons in these parasites.
Tips for Success
Other insights shared by Bates:
- Community cats should not be relocated. Many risk injury or death from vehicles or predators in their determination to travel miles to return to their colonies.
- Attempts to completely remove a cat colony will only result in another cat colony moving in and producing kittens, a phenomenon known as the vacuum effect.
- The best way to lure intact community cats into humane traps is to place traps where cats gather to eat and allow a few days for the cats to get used to them. Then create a trail of food leading into the traps and placing the highest-quality smelly food (to these cats, that is usually sardines or tuna or even Kentucky Fried Chicken) in the middle of the traps.
- If you find a homeless cat whose left ear is notched, do not bring him to a shelter unless he is injured or ill. This is the universal sign that he is a community cat who has been neutered.
- Do not leave bowls of food out; they attract raccoons and other wildlife. Set up specific feeding times and remove bowls within an hour.
Numbers indicate that this multi-approach effort is working. Before the TNVR program began in 2009, Palm Beach County shelters took in 19,000 homeless cats with more than 14,000 cats euthanized in 2008. That number has been cut to fewer than 2,000 cats euthanized this year in county shelters.
“It really takes a village to help these cats,” says Bates. “We have a passionate group of board members, staff, volunteers, and people in neighborhoods all doing their part to help feed and keep these cats healthy.”
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.
Arden Moore is The Pet Health and Safety Coach. She is a best-selling author, radio show host, in-demand speaker and master certified pet first aid/CPR instructor who travels the country teaching with Pet Safety Dog Kona and Pet Safety Cat Casey. Learn more at www.ardenmoore.com and www.facebook.com/ardenmoore.

Reducing fear, anxiety, and stress during visits and procedures takes time, teamwork, and sometimes a little experimentation. Here are three success stories shared by a veterinarian, trainer, and owner.
Tyson’s Turnaround
Tyson is a 12-year-old Schnauzer mix who first came to us last year for a wellness visit. The owner told us that his previous clinic had to muzzle him, and he was handled somewhat roughly. She wanted to get away from that. On his first visit we just got a feel for his comfort level. He barked and growled at us in the room but took treats willingly. He allowed an otoscopic exam but was tense, and when the stethoscope was introduced, he actively tried to bite. Approaching him with a muzzle sent him into a panic. We sent some Trazodone home with him that day for future visits and discussed doing a set of behavioral visits to help desensitize him to handling and instruments.
owner told us that his previous clinic had to muzzle him, and he was handled somewhat roughly. She wanted to get away from that. On his first visit we just got a feel for his comfort level. He barked and growled at us in the room but took treats willingly. He allowed an otoscopic exam but was tense, and when the stethoscope was introduced, he actively tried to bite. Approaching him with a muzzle sent him into a panic. We sent some Trazodone home with him that day for future visits and discussed doing a set of behavioral visits to help desensitize him to handling and instruments.
Tyson returned five months later for scheduled vaccinations. With Trazodone on board he was still on edge but performed tricks for us and approached us for treats. He allowed me to auscult him while he had treats to eat. This was great progress! We still decided to sedate for the remainder of his procedures to avoid backtracking on his progress.
Over the course of the next year Tyson’s owner took her own Fear Free steps at home, buying her own grooming table and clipping him herself. She was patient with him and even learned to Dremel his nails.
When it was nearly time for Tyson’s annual exam she set up behavioral sessions with us, so we could work on desensitization. We discovered Trazodone made him a little grumpy at home, so we switched to gabapentin, which worked well for him. On his first behavioral visit the difference was obvious. He came right up to staff for treats, did all of his tricks, and allowed us to touch him everywhere. We could feel his belly, touch his ears and legs, and look in his mouth. We started doing mock injections with a capped needle with no reaction. The only thing that still triggered him was obvious restraint.
For his annual wellness visit, Tyson allowed a full exam. We applied topical lidocaine at his injection sites and where we planned to draw blood for a heartworm test. We put a donut collar on Tyson prior to his vaccines as a precaution, and asked the owner to hold his harness to keep him steady (he was really into the treats and a bit wiggly). He did not react to his vaccinations and even held still long enough for us to get a blood draw from his back leg.
Tyson made a huge turnaround, and I think the owner’s willingness to do her part played a big role. It has been great to see the difference Fear Free techniques have made!
Susan Sappington, DVM, Rock Bridge Animal Hospital, Columbia, Missouri
Elke’s Excellent Experience
Elke had her annual veterinary checkup yesterday, and by doing some simple things we were able to make her visit less stressful and even a bit enjoyable. Our veterinarian is part of a Fear Free practice (Thank you, Animal Hospital of North Asheville) and embraces a cooperative care approach that allows animals to have choices and dictate the pace at which we move through the visit.
able to make her visit less stressful and even a bit enjoyable. Our veterinarian is part of a Fear Free practice (Thank you, Animal Hospital of North Asheville) and embraces a cooperative care approach that allows animals to have choices and dictate the pace at which we move through the visit.
In the photo, you see that there is a comfortable mat for Elke to use. Having a soft spot to rest on is so much nicer for dogs than just having the cold, hard floor. She was a bit nervous, so we created a treat search for her by hiding treats in the blanket and Kong. It is one of her favorite things to do, and sniffing is an activity that we know helps calm dogs. During the actual exam, all of us (veterinarian, veterinary technician, and myself) gave her treats each time a new body part was examined. While Elke does not love going to the veterinarian’s office, with cooperative care and the Fear Free method she was able to relax and have a calm visit.
Joann Rechtine, CPDT-KA, MS, MPH, RN, The Loose Leash Academy, Black Mountain, North Carolina
Roger’s Routine
 We were beside ourselves on how to handle taking Roger to the vet. We put him through basic obedience and advanced obedience classes twice to learn manners and how to act appropriately. He has done great in our home and in our families’ homes as we know how to handle his anxiety. In our vet’s office, though, Roger would go crazy as his anxiety shot through the roof from all the smells and people. Thanks to the Fear Free program and team at Frey Pet Hospital, Roger can feel safer and happier going to the vet now. We are thankful for Fear Free Way!
We were beside ourselves on how to handle taking Roger to the vet. We put him through basic obedience and advanced obedience classes twice to learn manners and how to act appropriately. He has done great in our home and in our families’ homes as we know how to handle his anxiety. In our vet’s office, though, Roger would go crazy as his anxiety shot through the roof from all the smells and people. Thanks to the Fear Free program and team at Frey Pet Hospital, Roger can feel safer and happier going to the vet now. We are thankful for Fear Free Way!
Nicole Schroeder, Cedar Rapids, Iowa
Kim Campbell Thornton is content manager for Fear Free Pets and is a Level 3 Fear Free Certified Professional. She has been writing about dogs, cats, wildlife, and marine life since 1985.
Pharmacologic Options for Veterinary Visit Anxiety: An Evidenced-Based Review
In this webinar, Julia Albright, DVM, DACVB, covers the various pharmacological treatments used for veterinary visit anxiety and reviews the evidence behind each of these options.
Dr. Albright will:
1. Discuss the need to address veterinary visit anxiety
2. Review the evidence behind the commonly used pharmacological treatment options
3. Present protocols for reducing veterinary visit anxiety
Sponsored by Zoetis Petcare.

Just as we have our own individual taste preferences, so do dogs and cats. And food can be the way to their hearts. Many Fear Free Certified veterinary practices and Fear Free veterinarians even offer “menus” and keep track in pets’ records of personal preferences.
Of course, many cats will do anything for tuna. And dogs love those hot dogs. Those statements won’t stop the pet press.
However, veterinarians and veterinary technicians can also think outside the treat box. Sometimes, just because it’s novel, a treat may be more enticing. Also, at home these items might be used for training or for animals needing a bit of an appetite boost (always only with veterinary approval).
Who knew, for example, that many cats have a thing for olives (no pits please) or marshmallows. Or that dogs, and not necessarily Australian Cattle Dogs, love Vegemite, an Australian food spread made from leftover brewers’ yeast extract with various vegetables and spices. Most Americans disdain Vegemite, but many dogs love the stuff.
With Fear Free founder Dr. Marty Becker contributing, here’s a list of 20 surprising treats:
- Anchovy paste
- Apple
- Baby food (without onion)
- Bananas
- Blueberries
- Bonito fish flakes (known as katsuobushi in Japanese cuisine)
- Braunschweiger
- Cheerios
- Cheez Whiz/Easy Cheese
- Churros (fried-dough pastry)—hold the chocolate sauce
- Green beans
- Liverwurst
- Marshmallow cream
- Mini marshmallows
- Olives (no pits)
- Peas
- Peanut Butter (avoid sugar-free peanut butters containing the artificial sweetener Xylitol, which is toxic to pets)
- Rice cakes (plain)
- Sardines (in pesto, in olive oil or in water)
- Vegemite
Remember to keep portion sizes small, appropriate for the size of the pet. You don’t want to send him home with a tummy ache!
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.
Steve Dale, CABC (certified animal behavior consultant), hosts two national pet radio shows and is on WGN Radio, Chicago. He’s a regular contributor/columnist for many publications, including CATSTER, Veterinary Practice News, and the Journal of the National Association of Veterinary Technicians in America. He’s appeared on dozens of TV shows, including Oprah, many Animal Planet Programs, and National Geographic Explorer. He has contributed to or authored many pet books and veterinary textbooks such as “The Cat: Clinical Medicine and Management” and co-edited Decoding Your Dog, by the American College of Veterinary Behaviorists. He speaks at conferences around the world. www.stevedale.tv.
Brain Games for Bed Rest
Fear Free proudly presents Force-Free Trainer Jessica Ring, CPDT-KA, CTC, PMCT, owner and operator of My Fantastic Friend in Ellicott City, MD. Following Dr. Rachel Abrams’ brief tips on managing post-surgical pain, Jessica discusses brain games and mental stimulation for canine patients who are on “bed rest.”

For Fear Free Certified veterinary professionals, job one is reducing fear, anxiety, and stress during visits and procedures. Here are three successful approaches to making the veterinary clinic a safe and happy space for pets!
Slaying Fiona’s Fear
 When Fiona first came to us at Gamble Pet Clinic, an examination without a fearful reaction from her was impossible. An attack by another dog at a young age had caused her to be anxious and nervous ever since. She had been muzzled at every veterinary clinic since her attack until coming to Gamble Pet Clinic. She was fearful initially, trying to nip at the doctor and staff when they attempted to examine her.
When Fiona first came to us at Gamble Pet Clinic, an examination without a fearful reaction from her was impossible. An attack by another dog at a young age had caused her to be anxious and nervous ever since. She had been muzzled at every veterinary clinic since her attack until coming to Gamble Pet Clinic. She was fearful initially, trying to nip at the doctor and staff when they attempted to examine her.
We began working with Fiona in an Elizabethan collar. When a pet is appropriately acclimated to it, an Elizabethan collar can be a great alternative to a muzzle because it allows the dog’s head, nose, and mouth to move naturally and easily while providing a barrier that keeps the patient and staff safe and comfortable. If used appropriately and only in a positive manner from the start, it can be a great tool for Fear Free work on anxious or stressed patients like Fiona. In this way, Dr. Gamble is able to examine Fiona while she is distracted by treats like cheese and pretzel sticks. Both Dr. Gamble and Samantha, her assistant, are Fear Free Certified, making the whole process go smoothly.
Fiona’s Fear Free journey continued with regular Victory Visits to the clinic where everyone worked slowly and calmly with her to get her used to the environment and build her trust. Gradually, her anxiety about coming to the clinic decreased and she started to see it as a positive experience, looking forward to the treats and trusting the doctor enough to begin letting her touch and examine her. Every time she comes in, we use Fear Free techniques that build on the foundation we have laid. Fiona is still working on her Fear Free process and we are working to gain her full trust. We are so proud of the amazing strides she has made with us so far in the Fear Free setting!
Emily Andrade, CVA, Fear Free Level 3 Certified, Gamble Pet Clinic, Fort Collins, Colorado
Networking News
 I took the Fear Free course. It was interesting and useful. I’m now working with two local veterinary offices who found me through the Fear Free website.
I took the Fear Free course. It was interesting and useful. I’m now working with two local veterinary offices who found me through the Fear Free website.
Getting the Fear Free certificate increased business this year more than any other marketing I’ve done. It seems that more veterinarians in my area are implementing Fear Free concepts in their practices and seeking trainers to partner with.
Delores Carter, MA, KPA CTP, UW-AAB, The Learning Dog Academy, Brighton, Michigan
A Blood Draw for Sal
 Sal was brought to us to establish why he had been having chronic vomiting and diarrhea. When I approached him in the lobby, he immediately pinned his ears and retreated under the couch. We brought him into an exam room, and he warmed up a bit but was still wary. Mom and Dad mentioned that in the past at other clinics he was taken to “the back” for vaccines and they could hear him vocalizing from the exam room.
Sal was brought to us to establish why he had been having chronic vomiting and diarrhea. When I approached him in the lobby, he immediately pinned his ears and retreated under the couch. We brought him into an exam room, and he warmed up a bit but was still wary. Mom and Dad mentioned that in the past at other clinics he was taken to “the back” for vaccines and they could hear him vocalizing from the exam room.
We needed to sedate him to further work up his history of vomiting and diarrhea. Since this would take a while, Mom and Dad went out for lunch and we kept Sal in our treatment area, where he became noticeably more anxious with the absence of his family. We used desensitization and counterconditioning techniques with small pieces of Braunschweiger and he eventually did not even notice when he was being touched along his epaxial muscles. He did not vocalize or notice whatsoever when we gave him his IM sedation. His abdominal ultrasound was normal, which was great for him but meant that we needed to further work up his symptoms. The veterinarian on the case recommended that he come in for an ACTH stimulation test.
The technician working with him mentioned that we needed to provide Sal with some pre-visit medications so it would be less stressful for him. This specific test measures cortisol and if Sal was stressed it could affect the test results. The veterinarian consulted our behavior department about what medications he could come in on that would not affect the test results.
Because Sal vomited during a trial of Trazodone at home, he came in on gabapentin alone. Because this didn’t go well, we called it a day and decided to attempt a different medication combination. The next time Sal received gabapentin, Trazodone, and Cerenia 30 minutes prior to the appointment time. This time when we entered the room, Sal was significantly sleepier and more relaxed. We offered him chicken baby food and he loved it. We placed him on the table, Mom and Dad talked to him and fed him while one technician occluded his vein, and the other technician performed the blood draw and administered the medication. Sal ate chicken baby food throughout the entire process. Then Mom and Dad waited patiently in the exam room with Sal until it was time to draw the 1-hour post sample. We repeated the same process. Sal was a rock star and ate throughout the blood draw. Now we have a set protocol for when he comes in for workups or annual visits, and he stays with mom and dad for any procedure possible.
Maria Marano, RVT, Fear Free Certified, Community Practice, The Ohio State University Veterinary Medical Center, Columbus, Ohio
Kim Campbell Thornton is content manager for Fear Free Pets and is a Level 3 Fear Free Certified Professional. She has been writing about dogs, cats, wildlife, and marine life since 1985.

Course Overview
Inadequate pain control can damage the human-animal bond and impede an animal’s ability to maintain normal function and to recover from injury or illness. This module will focus on the fundamentals in measurement and the scaling and scoring of pain, so that we can more effectively treat patients’ pain and suffering.
This course, approved for 1 RACE CE hour, was written by Dr. Ralph Harvey, DVM, MS, DACVA, UTCVM.
This course consists of five lessons:
- Lesson 1: Pain as a Vital Sign
- Lesson 2: Behavioral Signs of Pain
- Lesson 3: Scales and Scoring of Acute Pain
- Lesson 4: Evaluating Chronic Pain
- Lesson 5: Case Examples
This course is endorsed by the International Veterinary Academy of Pain Management.


Fear Free is a concept that benefits both animals and the people working with them. This is especially evident when the animal being cared for is of tremendous size and strength, such as the pig patients of Fear Free certified professional Dr. Alicia McLaughlin at The Center for Bird and Exotic Animal Medicine near Seattle, Washington.
“When pigs are stressed, they communicate their stress very clearly, both vocally and with their body language, which can be very upsetting for their family and veterinary staff. When pigs are less stressed, their families are more relaxed, and their veterinarian is able to provide better quality medical care,” says McLaughlin.
Handle With Care
Coercive handling causes increased tension for everyone. Forced handling is also likely to create fear memories and aversions that make the pig more challenging to work with and create a greater safety risk for both pig and people.
“Pigs are very touchy about their bodies. Many don’t like being touched unless they are being scratched in certain areas. If they feel that any handling attempts are coercive, they’re likely to react strongly and negatively,” says McLaughlin. “Most pigs have an extreme dislike for restraint, having their facial area handled, or being picked up. Forcing a pig to remain still with restraint even momentarily for sedation can cause tension for everyone. Many will vocalize in distress when this handling occurs; with squeal decibels rivaling those made by a fighter jet.”
Most pigs who come in are open to the veterinary experience if the staff interacts in a way that signals they are friendly, not threatening. Encouraging the pig’s willing participation during care using treat rewards, setting a soothing care environment, and using calming aids are all approaches resulting in less stress and greater success.
Reading Porcine Body Language
Rewards and food aren’t the only things that work to keep pigs calm during Fear Free care. Carefully observing the pig’s body language for signs of fear, anxiety, and stress (FAS) throughout care is also key for keeping the pig in a calmer, more amenable state and for keeping both pig and humans safe in the process.
Signs of FAS in pigs include muscles tensing, shying away, lowering the head, moving into a corner, or finding security by moving their body next to a wall. In some cases, FAS may be subtle, with one potential indicator being the pig coming up to take treats, but then retreating to a safe distance immediately after the interaction. Loud squeals and excessive vocalizations are audible signs of a pig’s distress.
When in a state of FAS, pigs will attempt to avoid the situation and move away or hide. If pushed, though, pigs on rare occasions may try to bite. Biting is rare, a last-ditch escape effort from pigs who are responding to the situation as if they’re going to die.
Sedation Can Help
It’s far better to note early signs of FAS and make ongoing adjustments to keep the pig calm than it is to risk escalation and the creation of fearful memories of the experience. Sedation isn’t a last resort for pig care, but a protective practice used early and often when it comes to reducing the FAS pigs experience. In many cases, full sedation is recommended to eliminate the distress and ensuing struggle that could otherwise occur if the pig becomes upset. But before jumping immediately to sedation, Dr. McLaughlin is careful to make the sedation itself as non-stressful and Fear Free as possible.
Sedating a pig can be tricky, especially since most pigs are averse to having their faces touched or to being held in place even momentarily. It’s important to Dr. McLaughlin to keep sedation minimally stressful. Oral pre-sedation medication, such as Valium that’s ground up and placed on food, can take the edge off before sedation. With pre-sedation medication on board, the pig is often calm enough to tolerate minimal restraint while a gas mask is placed over the face. No more than a minute later, the pig is out and ready to be cared for.
“Time pressures can result in handling and care being more coercive than we want it to be. There is something to getting it done quick and dirty. But there are long-term effects that go with that and it’s not my preference to do that,” says Dr. McLaughlin.
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.
Mikkel Becker, CBCC-KA, CPDT-KA, KPA CTP, CDBC, CTC, is lead animal trainer for Fear Free Pets. She is a certified behavior consultant and trainer who specializes in reward-based training that’s partnered closely with the pet’s veterinary team. Mikkel is coauthor of six books, including From Fearful to Fear Free.

We don’t like to be negative, but, well, you’re wrong. Here are the top 10 myths about the difficulty of earning Fear Free Practice Certification and what you might be surprised to learn about getting your practice certified.
- We don’t have separate cat and dog entrances.
Species-specific entrances are not required. If you have them, that is great! There is an optional standard for which you will score points for having them, but they are not a requirement.
- We don’t have a designated cat room.
A designated cat room is a plus, but it’s not a must. You can earn points for having one, but you won’t lose points for not having one.
- We can’t afford to pay for everyone’s memberships on top of Practice Certification.
Once a practice is certified, you pay only the annual Practice Certification dues; you no longer pay for individual members.
- We have to repaint the practice in Fear Free colors.
We don’t expect you to! If you are already planning to refresh the practice, it makes sense to pick some Fear Free colors, but it’s not a requirement.
- We are a Fear Free Practice already; every team member is certified.
Congratulations on getting everyone certified! However, to be an official Fear Free Certified Practice, you must complete the Practice Certification process. Chances are you will save money!
- Not everyone in the practice is Fear Free Certified.
To be eligible for Practice Certification, only 25 percent of your staff must be Fear Free CertifiedÒ with an active membership.
- The standards aren’t available to review prior to applying.
Members can download and begin implementing the Standards and Supporting Examples at any time.
- We don’t have room for separate dog and cat waiting areas.
Separate waiting areas are not required, though visual blocks are encouraged if clients and patients are unable to wait outside or be moved straight into an exam room.
- Our scrubs aren’t in “Fear Free-approved” colors.
Team members of Fear Free Certified Practices are not required to wear any specific-colored scrubs or lab coats.
- The process is too difficult.
Practice Certification is a commitment, but it is worth it.
For more information, learn more at fearfreepets.com/practice-certification.
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.