Course Overview
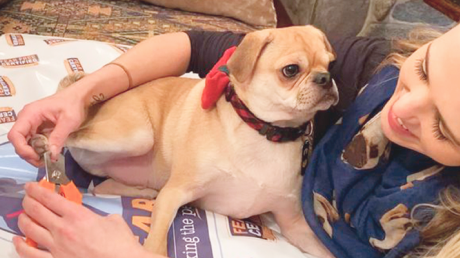
For humans, nail trims are mundane experiences. But for pets, nail care can cause stress by imposing on their personal space, restricting their freedom to move, and sometimes causing discomfort or even pain.
Successful nail care encompasses more than just being able to physically maintain nails. True success is found in gaining calm participation and trust from the animals you’re working with.
This course will teach you to:
- View nail care from the pet’s perspective and identify several common causes of FAS
- Understand the uses, benefits and drawbacks of each common nail trim tool: clippers, nail grinders, nail files, and scratch boards
- Incorporate the Fear Free concepts of Gentle Control, Considerate Approach and touch gradient into nail care
- Describe how, and just as importantly, when, to use food distractions, desensitization and classical conditioning, or consider medications to achieve Fear Free nail trims
This one-hour course is open to all professionals who are signed up for a Fear Free certification program and is approved for 1 RACE CE hour and one hour of CEUs from CCPDT, IAABC and KPA
This course consists of four lessons:
- Lesson 1: Nails, from the Pet’s Perspective
- Lesson 2: Tools of the Trade
- Lesson 3: Applying Fear Free Core Concepts to Nail Care
- Lesson 4: Going Beyond Food Distractions

Just as we have our own individual taste preferences, so do dogs and cats. And food can be the way to their hearts. Many Fear Free Certified veterinary practices and Fear Free veterinarians even offer “menus” and keep track in pets’ records of personal preferences.
Of course, many cats will do anything for tuna. And dogs love those hot dogs. Those statements won’t stop the pet press.
However, veterinarians and veterinary technicians can also think outside the treat box. Sometimes, just because it’s novel, a treat may be more enticing. Also, at home these items might be used for training or for animals needing a bit of an appetite boost (always only with veterinary approval).
Who knew, for example, that many cats have a thing for olives (no pits please) or marshmallows. Or that dogs, and not necessarily Australian Cattle Dogs, love Vegemite, an Australian food spread made from leftover brewers’ yeast extract with various vegetables and spices. Most Americans disdain Vegemite, but many dogs love the stuff.
With Fear Free founder Dr. Marty Becker contributing, here’s a list of 20 surprising treats:
- Anchovy paste
- Apple
- Baby food (without onion)
- Bananas
- Blueberries
- Bonito fish flakes (known as katsuobushi in Japanese cuisine)
- Braunschweiger
- Cheerios
- Cheez Whiz/Easy Cheese
- Churros (fried-dough pastry)—hold the chocolate sauce
- Green beans
- Liverwurst
- Marshmallow cream
- Mini marshmallows
- Olives (no pits)
- Peas
- Peanut Butter (avoid sugar-free peanut butters containing the artificial sweetener Xylitol, which is toxic to pets)
- Rice cakes (plain)
- Sardines (in pesto, in olive oil or in water)
- Vegemite
Remember to keep portion sizes small, appropriate for the size of the pet. You don’t want to send him home with a tummy ache!
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.
Steve Dale, CABC (certified animal behavior consultant), hosts two national pet radio shows and is on WGN Radio, Chicago. He’s a regular contributor/columnist for many publications, including CATSTER, Veterinary Practice News, and the Journal of the National Association of Veterinary Technicians in America. He’s appeared on dozens of TV shows, including Oprah, many Animal Planet Programs, and National Geographic Explorer. He has contributed to or authored many pet books and veterinary textbooks such as “The Cat: Clinical Medicine and Management” and co-edited Decoding Your Dog, by the American College of Veterinary Behaviorists. He speaks at conferences around the world. www.stevedale.tv.
Brain Games for Bed Rest
Fear Free proudly presents Force-Free Trainer Jessica Ring, CPDT-KA, CTC, PMCT, owner and operator of My Fantastic Friend in Ellicott City, MD. Following Dr. Rachel Abrams’ brief tips on managing post-surgical pain, Jessica discusses brain games and mental stimulation for canine patients who are on “bed rest.”

For Fear Free Certified veterinary professionals, job one is reducing fear, anxiety, and stress during visits and procedures. Here are three successful approaches to making the veterinary clinic a safe and happy space for pets!
Slaying Fiona’s Fear
 When Fiona first came to us at Gamble Pet Clinic, an examination without a fearful reaction from her was impossible. An attack by another dog at a young age had caused her to be anxious and nervous ever since. She had been muzzled at every veterinary clinic since her attack until coming to Gamble Pet Clinic. She was fearful initially, trying to nip at the doctor and staff when they attempted to examine her.
When Fiona first came to us at Gamble Pet Clinic, an examination without a fearful reaction from her was impossible. An attack by another dog at a young age had caused her to be anxious and nervous ever since. She had been muzzled at every veterinary clinic since her attack until coming to Gamble Pet Clinic. She was fearful initially, trying to nip at the doctor and staff when they attempted to examine her.
We began working with Fiona in an Elizabethan collar. When a pet is appropriately acclimated to it, an Elizabethan collar can be a great alternative to a muzzle because it allows the dog’s head, nose, and mouth to move naturally and easily while providing a barrier that keeps the patient and staff safe and comfortable. If used appropriately and only in a positive manner from the start, it can be a great tool for Fear Free work on anxious or stressed patients like Fiona. In this way, Dr. Gamble is able to examine Fiona while she is distracted by treats like cheese and pretzel sticks. Both Dr. Gamble and Samantha, her assistant, are Fear Free Certified, making the whole process go smoothly.
Fiona’s Fear Free journey continued with regular Victory Visits to the clinic where everyone worked slowly and calmly with her to get her used to the environment and build her trust. Gradually, her anxiety about coming to the clinic decreased and she started to see it as a positive experience, looking forward to the treats and trusting the doctor enough to begin letting her touch and examine her. Every time she comes in, we use Fear Free techniques that build on the foundation we have laid. Fiona is still working on her Fear Free process and we are working to gain her full trust. We are so proud of the amazing strides she has made with us so far in the Fear Free setting!
Emily Andrade, CVA, Fear Free Level 3 Certified, Gamble Pet Clinic, Fort Collins, Colorado
Networking News
 I took the Fear Free course. It was interesting and useful. I’m now working with two local veterinary offices who found me through the Fear Free website.
I took the Fear Free course. It was interesting and useful. I’m now working with two local veterinary offices who found me through the Fear Free website.
Getting the Fear Free certificate increased business this year more than any other marketing I’ve done. It seems that more veterinarians in my area are implementing Fear Free concepts in their practices and seeking trainers to partner with.
Delores Carter, MA, KPA CTP, UW-AAB, The Learning Dog Academy, Brighton, Michigan
A Blood Draw for Sal
 Sal was brought to us to establish why he had been having chronic vomiting and diarrhea. When I approached him in the lobby, he immediately pinned his ears and retreated under the couch. We brought him into an exam room, and he warmed up a bit but was still wary. Mom and Dad mentioned that in the past at other clinics he was taken to “the back” for vaccines and they could hear him vocalizing from the exam room.
Sal was brought to us to establish why he had been having chronic vomiting and diarrhea. When I approached him in the lobby, he immediately pinned his ears and retreated under the couch. We brought him into an exam room, and he warmed up a bit but was still wary. Mom and Dad mentioned that in the past at other clinics he was taken to “the back” for vaccines and they could hear him vocalizing from the exam room.
We needed to sedate him to further work up his history of vomiting and diarrhea. Since this would take a while, Mom and Dad went out for lunch and we kept Sal in our treatment area, where he became noticeably more anxious with the absence of his family. We used desensitization and counterconditioning techniques with small pieces of Braunschweiger and he eventually did not even notice when he was being touched along his epaxial muscles. He did not vocalize or notice whatsoever when we gave him his IM sedation. His abdominal ultrasound was normal, which was great for him but meant that we needed to further work up his symptoms. The veterinarian on the case recommended that he come in for an ACTH stimulation test.
The technician working with him mentioned that we needed to provide Sal with some pre-visit medications so it would be less stressful for him. This specific test measures cortisol and if Sal was stressed it could affect the test results. The veterinarian consulted our behavior department about what medications he could come in on that would not affect the test results.
Because Sal vomited during a trial of Trazodone at home, he came in on gabapentin alone. Because this didn’t go well, we called it a day and decided to attempt a different medication combination. The next time Sal received gabapentin, Trazodone, and Cerenia 30 minutes prior to the appointment time. This time when we entered the room, Sal was significantly sleepier and more relaxed. We offered him chicken baby food and he loved it. We placed him on the table, Mom and Dad talked to him and fed him while one technician occluded his vein, and the other technician performed the blood draw and administered the medication. Sal ate chicken baby food throughout the entire process. Then Mom and Dad waited patiently in the exam room with Sal until it was time to draw the 1-hour post sample. We repeated the same process. Sal was a rock star and ate throughout the blood draw. Now we have a set protocol for when he comes in for workups or annual visits, and he stays with mom and dad for any procedure possible.
Maria Marano, RVT, Fear Free Certified, Community Practice, The Ohio State University Veterinary Medical Center, Columbus, Ohio
Kim Campbell Thornton is content manager for Fear Free Pets and is a Level 3 Fear Free Certified Professional. She has been writing about dogs, cats, wildlife, and marine life since 1985.

Six Client Tips for Puppy Socialization
Veterinarians often recommend that new puppy owners actively socialize their puppy during the sensitive socialization period. Well-intentioned pet parents may take that general guidance and inadvertently create, not prevent, problems. In this webinar, Jacqueline Neilson, DVM, DACVB, demonstrates how sharing six socialization principles will allow veterinary staff to help owners make wise choices for socialization that promote the pups’ emotional and physical wellbeing.
Sponsored by Elanco.

For humans, overcoming fear, or at least learning to deal with it, takes time and practice. That’s even more true for pets, because we can’t communicate that veterinary exams and procedures will help them to feel better or stay healthy. Fortunately, Fear Free techniques can help to send the message to pets that they don’t need to be afraid, and Fear Free education can help humans better understand their animals’ fears and needs.
Happy Hunter
 Hunter, a 2-year-old mixed breed, enjoys looking out the windows in the lobby of our clinic. By starting his visit there, asking his mom questions and listening to his heart and lungs, we can make sure he is comfortable enough to continue his exam in the exam room. But it was a different story when he first came in almost two years ago. Because of a previous frightening experience at another clinic, he was wary of us and the handling and procedures being done. He would bare his teeth, growl, and even try to nip at Dr. Gamble’s hands when she tried to touch him. Through consistent Victory Visits, pre-visit training and medications, and desensitization to areas where vaccines and other needle pokes are typically given, we are now able to provide him and his owner with a comfortable and rewarding experience every time he is in. Now he sits patiently and lets Dr. Gamble examine him—with the help of some cheese and marshmallows, not to mention smears of his favorite treats, peanut butter and canned food. During Hunter’s victory visits, we commonly work on the desensitization process without actually following through with an injection. “Happy visits, along with some training classes and behavior work on our part, have made a world of difference to Hunter,” writes his owner, Beth. “Hunter is now excited to see Emily, Heather, Dr. Gamble, and many other staff members as soon as he walks through the front door. He is a much happier dog at the vet thanks to Gamble Pet Clinic’s Fear Free work.”
Hunter, a 2-year-old mixed breed, enjoys looking out the windows in the lobby of our clinic. By starting his visit there, asking his mom questions and listening to his heart and lungs, we can make sure he is comfortable enough to continue his exam in the exam room. But it was a different story when he first came in almost two years ago. Because of a previous frightening experience at another clinic, he was wary of us and the handling and procedures being done. He would bare his teeth, growl, and even try to nip at Dr. Gamble’s hands when she tried to touch him. Through consistent Victory Visits, pre-visit training and medications, and desensitization to areas where vaccines and other needle pokes are typically given, we are now able to provide him and his owner with a comfortable and rewarding experience every time he is in. Now he sits patiently and lets Dr. Gamble examine him—with the help of some cheese and marshmallows, not to mention smears of his favorite treats, peanut butter and canned food. During Hunter’s victory visits, we commonly work on the desensitization process without actually following through with an injection. “Happy visits, along with some training classes and behavior work on our part, have made a world of difference to Hunter,” writes his owner, Beth. “Hunter is now excited to see Emily, Heather, Dr. Gamble, and many other staff members as soon as he walks through the front door. He is a much happier dog at the vet thanks to Gamble Pet Clinic’s Fear Free work.”
Emily Andrade, CVA, Fear Free Level 3 Certified, Gamble Pet Clinic, Fort Collins, Colorado
Fear Free Education Win
 Recently, there was an event called Woof Fest held during a downtown pub crawl. Our clinic sponsored “Dog Trivia,” and I focused the questions on a pet’s emotional health, such as “Is this dog’s body language calm or stressed?” and “A dog wagging their tail is always happy. True or False?” Hundreds of people played our trivia game, and it was such a rewarding experience to educate the public on the topic.
Recently, there was an event called Woof Fest held during a downtown pub crawl. Our clinic sponsored “Dog Trivia,” and I focused the questions on a pet’s emotional health, such as “Is this dog’s body language calm or stressed?” and “A dog wagging their tail is always happy. True or False?” Hundreds of people played our trivia game, and it was such a rewarding experience to educate the public on the topic.
Natalie Gruchow, CVPM, Animal Health Clinic, Fargo, North Dakota
Sammy’s Success
 Sammy had grown up in a hoarding situation and was fearful at the time of his adoption. Unless he was sedated, the six-year-old dog would bark and lunge or even eliminate from fear during veterinary visits. A prescription for an SSRI helped and the team tried additional medications at different doses, but Sammy would push through the medications and continue to show fear aggression. At first, he was unable to generalize that humans weren’t scary, so it was important for him to see the same person at the hospital on each visit. That wasn’t easy, but eventually the right person came along who was able to take the time and effort for Sammy to become comfortable. It took six months of Victory Visits spent eating chicken, practicing chin rests and lying on his side, and undergoing desensitization to having his leg shaved, the scent of alcohol, application of a topical product for numbness, and the pretend poke of a needle, but in July Sammy underwent his first successful blood draw. Now we are routinely doing happy visits to keep the momentum going.
Sammy had grown up in a hoarding situation and was fearful at the time of his adoption. Unless he was sedated, the six-year-old dog would bark and lunge or even eliminate from fear during veterinary visits. A prescription for an SSRI helped and the team tried additional medications at different doses, but Sammy would push through the medications and continue to show fear aggression. At first, he was unable to generalize that humans weren’t scary, so it was important for him to see the same person at the hospital on each visit. That wasn’t easy, but eventually the right person came along who was able to take the time and effort for Sammy to become comfortable. It took six months of Victory Visits spent eating chicken, practicing chin rests and lying on his side, and undergoing desensitization to having his leg shaved, the scent of alcohol, application of a topical product for numbness, and the pretend poke of a needle, but in July Sammy underwent his first successful blood draw. Now we are routinely doing happy visits to keep the momentum going.
Beth Friedman, Canine Companion Consulting, Fort Collins, Colorado
Down Under Wonder
 Bruno is a goofy 8-year-old Bull Arab Cross (a type of Australian working dog). He has always been very friendly at the vet, but once pats stopped and the examination started, he would become suspicious and communicate his discomfort with aggressive behavior. Fortunately, Bruno’s owner has been committed to training. They had private training sessions and attended a Ready, Vet, Go! course. As part of Bruno’s training we incorporated a lot of owner education on subtle body language changes, as well as start and stop cues for Bruno. Bruno was trained with a sustained chin target, using a towel on a chair, as his start cue, meaning “I’m ready for procedure.” If he lifted his head, we immediately stopped the procedure. Bruno was also trained to be comfortable with a Baskerville Ultra Muzzle. We spent time teaching Bruno specific body parts such as tail, ear, and scruff, so that he knew what was about to happen. Over time we were able to pair several good vet clinic experiences (training on a Sunday in clinic) with lots of his fave foods, body scratches, and games. We also introduced veterinary equipment, including syringes, blunt needle, alcohol swabs, and stethoscope. When we weren’t actively training, he was taught a default “chill” behavior and rewarded for relaxed head, tail, and big breaths. He had several socialization visits at the vet, and when he required surgery for a lump removal we did practice runs with pre-visit medication to see what would work best for him. A planned course of action on admission saw him anesthetized as soon as possible to limit buildup of anxiety. Since then Bruno has had further training sessions and socializing vet visits. Recently he had his vaccinations and we were able to give his injection without any restraint by utilizing his muzzle and target training. Bruno is a great example of what teamwork can achieve when you have a committed owner and a Fear Free-trained vet and trainer, not to mention a goofy, food-motivated dog!
Bruno is a goofy 8-year-old Bull Arab Cross (a type of Australian working dog). He has always been very friendly at the vet, but once pats stopped and the examination started, he would become suspicious and communicate his discomfort with aggressive behavior. Fortunately, Bruno’s owner has been committed to training. They had private training sessions and attended a Ready, Vet, Go! course. As part of Bruno’s training we incorporated a lot of owner education on subtle body language changes, as well as start and stop cues for Bruno. Bruno was trained with a sustained chin target, using a towel on a chair, as his start cue, meaning “I’m ready for procedure.” If he lifted his head, we immediately stopped the procedure. Bruno was also trained to be comfortable with a Baskerville Ultra Muzzle. We spent time teaching Bruno specific body parts such as tail, ear, and scruff, so that he knew what was about to happen. Over time we were able to pair several good vet clinic experiences (training on a Sunday in clinic) with lots of his fave foods, body scratches, and games. We also introduced veterinary equipment, including syringes, blunt needle, alcohol swabs, and stethoscope. When we weren’t actively training, he was taught a default “chill” behavior and rewarded for relaxed head, tail, and big breaths. He had several socialization visits at the vet, and when he required surgery for a lump removal we did practice runs with pre-visit medication to see what would work best for him. A planned course of action on admission saw him anesthetized as soon as possible to limit buildup of anxiety. Since then Bruno has had further training sessions and socializing vet visits. Recently he had his vaccinations and we were able to give his injection without any restraint by utilizing his muzzle and target training. Bruno is a great example of what teamwork can achieve when you have a committed owner and a Fear Free-trained vet and trainer, not to mention a goofy, food-motivated dog!
Jacqui Johnston, Holland Park and Carina Vet Clinics and Trish Allan, All Pets Education and Training, Brisbane, Australia
Kim Campbell Thornton is content manager for Fear Free Pets and is a Level 3 Fear Free Certified Professional. She has been writing about dogs, cats, wildlife, and marine life since 1985.

Rachel Lees RVT, KPA CTP, VTS (Behavior)
A variety of animal training programs appear on cable and streaming networks. Some of the concepts depicted in these programs are appropriate for veterinary behavior cases and some are questionable. This article is not written to insult any of these programs, trainers, or networks but instead to discuss the learning theory and training philosophies demonstrated and review why veterinary behavior professionals are using alternative protocols.
Whether you are a veterinary team member working in general practice or are interested in behavior, it is important to recommend the most Fear Free and up-to-date information for patients and clients. Giving outdated information can potentially damage the human-animal bond between client and patient, potentially ending with the patient being rehomed or in some cases euthanized.
Punishment: May the Odds Be in Your Favor
Punishment is a technique used to weaken a behavior. For a stimulus to be “punishing,” the learner must find that stimulus aversive or undesirable enough to eliminate the behavior. Punishment is difficult to use properly and does not teach the learner to perform the correct behavior. Most important, using punishment can be a liability for veterinary professionals recommending this technique because it can put the safety of the owners and pets at risk.
The American Veterinary Society of Animal Behavior’s position statement on punishment reviews the many side effects of using this training method. Using remote punishment collars as well as choke and prong collars can cause physical damage such as damage to the skin, neck, and trachea area, an increase in intraocular pressure, upper airway obstruction, and nerve damage. For punishment to be effective, it must provoke a fear response from the learner, which can unfortunately be generalized to other stimuli in the learning environment. Consequently, this can make the animal become more fearful, anxious, and stressed in these contexts and situations.
Take the owner who is walking down the street with a 7-month-old Labrador Retriever puppy. The puppy shows a loose posture, wide tail wag, and becomes excitable on seeing people, sometimes jumping. For the owner, the dog’s jumping is undesirable. The trainer suggests using a remote “shock” collar for this issue. The owner is coached to shock the puppy for any jumping when interacting with people. The handler may be specifically punishing the pet for one behavior (jumping), but the puppy may begin to be concerned when people approach him because when this occurs, he receives a shock.
In the above example, the puppy may begin to show fear, anxiety, or stress with the approach of unfamiliar people. Using punishment, there is a risk that the learner (puppy) will associate the punishment (shock) with people approaching instead of the punishment (shock) being associated with the unwanted behavior (jumping on people).
Punishment needs to occur within 0.5 seconds of the start of the undesirable behavior. Therefore, the puppy would have to be shocked the moment his shoulders start to lower in anticipation of jumping to associate the punishment with the jumping behavior. Even with perfect timing, there is still a risk that the puppy may not associate the punishment with jumping.
Punishment Fails
Punishment can work to eliminate unwanted behaviors. The challenge is that it does not eliminate the motivation or give the learner a more appropriate behavior to perform.
In another instance, an owner was coached to use a remote collar to eliminate growling and aggression toward family members. If a family member approached the dog while he was eating a coveted bone and the dog growled, the family member was to correct the dog immediately with a shock. The growling behavior may be reduced, but it does not change the anxiety and concern related to the bone. The owners have now given the dog information that the approach of the owner is associated with a shock, which can increase the pet’s anxiety, fear, and stress. Long term, the pet may suddenly display with aggression but give only limited warning signs because the signals were suppressed with the remote collar. The animal was, in effect, told not to give this information. This makes this specific patient more dangerous and could put the family at greater risk.
In the above situation, the growling behavior is not a desirable response, but to the dog it was probably completely appropriate; he communicated his anxiety regarding the owner’s approach. Using punishment made that specific pet more dangerous. Avoiding these situations and confrontations are the first step in addressing this issue. A veterinary behaviorist may recommend specific behavior modification to change the way the pet feels during this interaction.
Veterinary behaviorists recommend that animal training should focus on setting up the environment, so the pet is more likely to perform desired behaviors, reinforcing desired behaviors, removing the reinforcer for undesirable behaviors, and addressing the emotional state of the learner. The use of punishment can slow learning, suppress behavior, increase fear and fear-based aggression, create damaging and unintended associations with owners and other environmental stimuli, and damage the human-animal bond.
Even though these techniques may be seen on TV, remember that you are the veterinary professional and your clients value your opinion and recommendations. Giving them the most up-to-date information regarding behavioral training can be lifesaving. Observe training classes that you may recommend to confirm that they use recommended Fear Free techniques. For more information, see resources from AVSAB on “Finding a Trainer” as well as the “Position Statement on Use of Punishment.” The Fear Free Level 3 course for professionals provides the tools to address typical dog and cat behaviors using Fear Free methods.
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.
Rachel Lees, a Level 3 Fear Free Certified Professional, is a veterinary technician specialist in behavior, a KPA certified training partner, and lead veterinary behavior technician at The Behavior Clinic in Olmsted Falls, Ohio. She loves helping people create and maintain a strong human-animal bond.

Canine Allergic Dermatitis: Creating a Higher Quality of Life for Everyone Involved
What better way to decrease stress than by increasing quality of life? In this webinar, Dana Liska, DVM, DACVD, expands the discussion surrounding canine allergic dermatitis and the stress chronic disease causes for dogs and for owners and veterinarians caring for them. She looks at data supporting an improved quality of life for everyone involved in the veterinarian-client-patient relationship.
Sponsored by Zoetis Petcare.

Canine Allergic Dermatitis: Creating a Higher Quality of Life for Everyone Involved
What better way to decrease stress than by increasing quality of life? In this webinar, Dana Liska, DVM, DACVD, expands the discussion surrounding canine allergic dermatitis and the stress chronic disease causes for dogs and for owners and veterinarians caring for them. She looks at data supporting an improved quality of life for everyone involved in the veterinarian-client-patient relationship.
Sponsored by Zoetis Petcare.

Kitten Socialization: Do Kittens Need Kindergarten?
Getting kittens off to a good start lays the foundation for an adulthood free of fear, anxiety, and stress. But just what does a “good start” mean? What exactly is kitten socialization? What role does genetics play, and what should we be doing for our kitten patients? In this webinar, Dr. Krista Sirois answers these questions and discuss the benefits of establishing a Kitty Kindergarten program in your clinic for your patients, pet parents, and your team.